Researcher discovers apt cure for treatment-resistant hypothyroidism
October 16, 2018 | Tuesday | News
Novel coordination of thyroid hormone with zinc promotes slow release of active hormone to supplement standard therapy
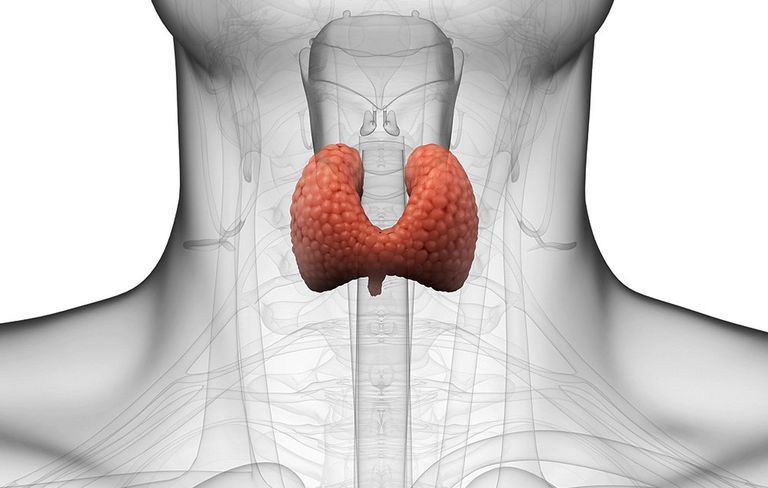
A new "metal-coordinated" drug-delivery technology potentially could be used to supplement the standard therapy for hypothyroidism, which affects nearly 10 million Americans, and many more patients worldwide, according to results of a study published in the journal Thyroid this month.
Researchers at Rush University Medical Centre have been pursuing an improved treatment for the minority of hypothyroid patients who don't respond well to the standard therapy. Now, their investigations into the way thyroid hormones given in tablets are absorbed and metabolized by the body suggest that a metal-coordinated molecule could prove to be a more effective therapy for all hypothyroid patients, according to Dr. Antonio Bianco.
He is a professor of medicine at the University of Chicago who was formerly a researcher and clinician at Rush, where the work detailed in the Thyroid paper was completed.
The new drug, poly-zinc-liothyronine (PZL), worked well in laboratory studies, Bianco said. Safety tests in animals and clinical trials in humans must still be conducted, and funding must be obtained to support that work. If all goes well, though, PZL could be offered to patients in only a few years, according to Bianco.
"We know enough about thyroid physiology in rats and humans that we feel confident that this drug is ready for prime time" in terms of working as well in humans as it has in the lab, he said.
The standard treatment for hypothyroidism is levothyroxine (L-T4), a synthetic version of the thyroid hormone thyroxine (T4), which in a healthy person is secreted by the thyroid gland. However, about 10 to 15 percent of L-T4-treated patients continue to have symptoms of the condition when treated, including weight gain, fatigue, lethargy, mood fluctuations, and problems with memory.
While investigating why minorities of hypothyroid patients still have symptoms even while adhering to the standard L-T4 therapy, these investigators discovered that, in rat models, a steady supply of liothyronine (L-T3) is necessary to "normalize" functional thyroid levels in the blood, and in such tissue areas as the brain, muscles and liver. That discovery gave new urgency to the hunt for a way to effectively deploy L-T3 over time in patients with hypothyroidism.
"A sustained-release L-T3 has been sort of the Holy Grail" in the field, Bianco said -- specifically, one that would perform well in clinical trials. PZL appears to solve that key problem and could be used in combination therapy. Bianco said. "When you take L-T3 alone, it's immediately absorbed. PZL isn't."
With PZL, T3 levels in the blood are "sustained over time with a delayed, but more desirable biological response," the study reported. As a result, PZL "minimizes post-dose peaks in circulating T3 typically seen with L-T3 administration." In other words, not only is PZL effective, but it also is less of a shock to the body.
If [PZL] is deemed to be safe and ready for clinical trial in humans, such trials can help determine if combination therapy can improve the signs and symptoms of hypothyroidism.