Can AI Become India’s Stethoscope?
October 31, 2025 | Friday | News
Disruptive Tech Takes Center Stage Through Health Innovation: The PIC–Wipro Roadmap
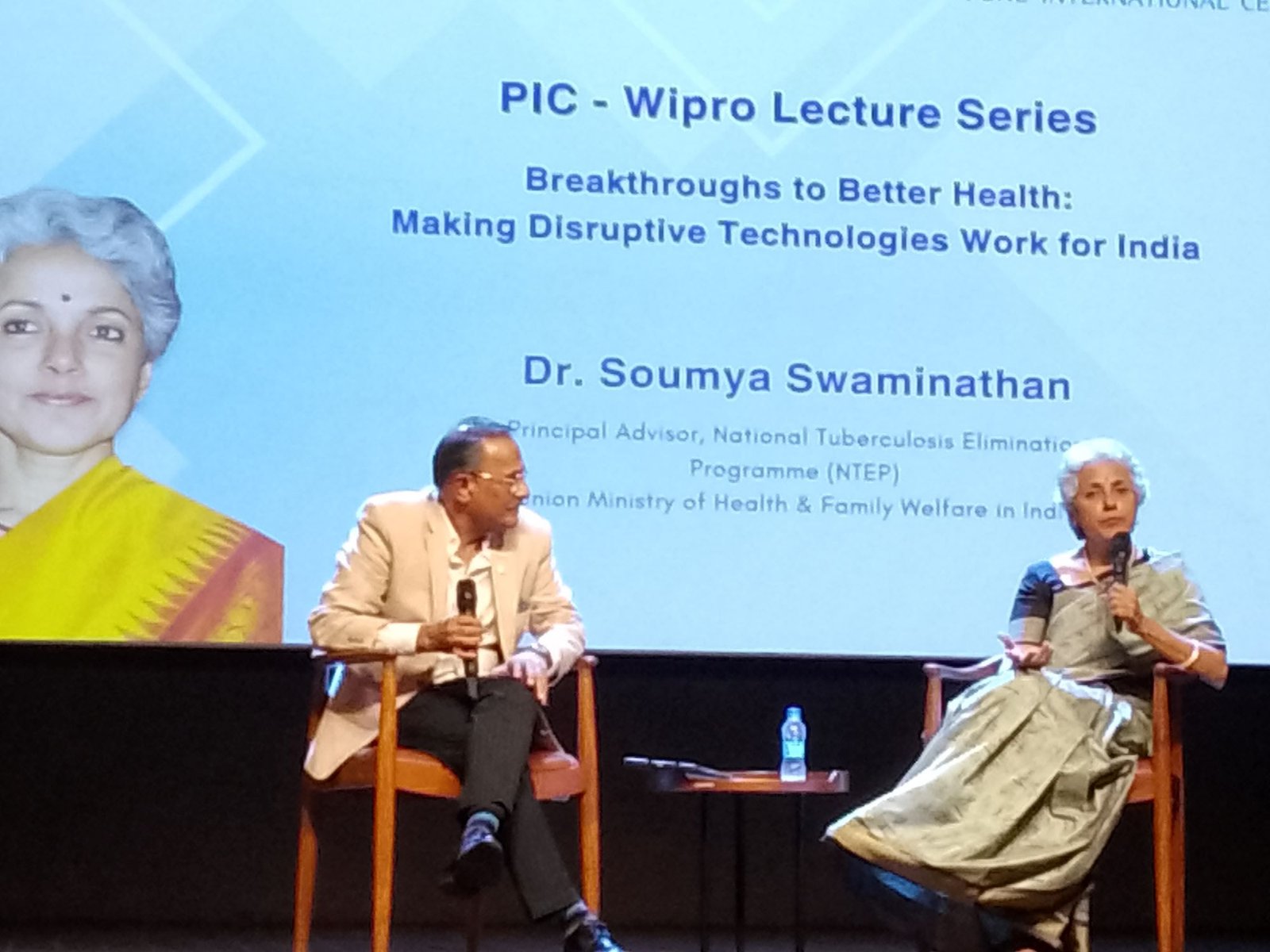
India stands on the cusp of a healthcare transformation defined not by incremental upgrades, but by disruptive technologies engineered for access, equity, and scale. This conviction underscored the latest session of the Pune International Centre (PIC)–Wipro Lecture Series titled “Breakthroughs to Better Health: Making Disruptive Technologies Work for India”, delivered by Dr Soumya Swaminathan — Principal Advisor, National Tuberculosis Elimination Program, Union Ministry of Health and Family Welfare — and attended by healthcare, technology, and policy leaders at Pune International Centre.
Speaking at the session, P.S. Narayan, Global Head – Sustainability & Social Initiatives at Wipro, emphasised that the company’s commitment to societal impact draws from the values enshrined in the Indian Constitution. He highlighted Wipro’s partnership with the Pune International Centre as a strategic collaboration centered on climate action, urban advancement, and public well-being, with technology — especially artificial intelligence — enabling scalable change. Public engagement in science, Narayan warned, is essential to ensure citizens become active shapers of technology, not passive consumers.
Major General Nitin Gadkari, Director, Pune International Centre, alongside Dr R.A. Mashelkar, President, PIC and Dr Vijay Kelkar, Vice President, PIC welcomed the audience and introduced Dr. Soumya Swaminathan as a leader who has built rare bridges between frontier research and population-scale health programmes.
Dr Soumya set the global context starkly: the leading cause of death in 2021 was COVID-19; by 2023, ischemic heart disease had resurged. Today, heat stress — driven by climate change — is claiming more lives worldwide, signaling how environmental disruption and health emergencies are now tightly interlocked. India faces a twin paradox — the South grappling with surging diabetes and metabolic disorders, while the North continues to battle malnutrition. Progress in maternal and child health has been hard-won, yet chronic illnesses such as cancer and diabetes are rising sharply. “Global risks are escalating and converging — economic shocks, geopolitics, and climate crises now manifest as health crises,” she cautioned, citing a world where the Amazon rainforest has become a net emitter of carbon and fossil-fuel subsidies still eclipse renewable investments.
Deadly infectious threats have not receded. Emerging pathogens of concern include Betacoronaviruses, Filoviruses, and Bunyaviruses, alongside the growing challenge of antimicrobial resistance. AMR alone is linked to 4.95 million deaths globally, including 1.27 million due to resistant bacteria — a silent pandemic. Non-communicable killers are equally alarming: air pollution now extends its harm to cognitive decline, while dietary risks — processed foods high in salt, sugar, and unhealthy fats — are reshaping the disease landscape. India is already home to 11.4 per cent diabetes prevalence and 15.3 per cent pre-diabetes, disproportionately concentrated in cities and southern states. By 2050, nearly 300 million Indians will be above 65, placing immense pressure on geriatric and primary healthcare systems. Meanwhile, fragmented care and variable quality cost 2.4 million lives every year — a reminder that inequality is a public-health crisis.
Dr Soumya argued that a technology is truly disruptive only if it makes healthcare more affordable, more accessible, and more efficient — not just technologically advanced. She showcased emerging breakthroughs rapidly reshaping medicine. mRNA platforms enabled the fastest vaccine response in history during COVID-19 and are now being repurposed for cancer, TB, malaria, and autoimmune diseases. Prototype-pathogen research aims to accelerate vaccine development by anticipating outbreaks rather than reacting to them.
Artificial Intelligence, described as “the stethoscope of the 21st century,” is now predicting heart attacks from ECGs, detecting Alzheimer’s from retinal scans, and improving tuberculosis diagnostics with high precision. AlphaFold, the AI platform recently honored with a Nobel Prize recognition, has redrawn the boundaries of protein science. Indian innovations — including Swaasa for respiratory health and Garbhini-GA2, the country’s first indigenous AI model for pregnancy dating — represent technological sovereignty in health intelligence.
Wearables and remote monitoring promise to shift care from hospitals to homes, while biome-based therapies open radical new possibilities for metabolic diseases. Breakthroughs such as neurotech-enabled communication for paralysed individuals signal the start of a bio-hybrid revolution. Simple but powerful inventions like the BEMPU Bracelet — detecting neonatal hypothermia in low-resource settings — demonstrate that innovation is as much about empathy as engineering. At the same time, frontier tools such as gene drive technologies demand rigorous ethical governance, particularly in biodiversity-rich, climate-sensitive countries like India.
Digital health infrastructure has advanced rapidly with the Ayushman Bharat Digital Mission. As of August 5, 2025, over 79.91 crore Ayushman Bharat Health Accounts (ABHAs) — nearly 800 million unique digital identities — have been generated, unlocking unprecedented portability and continuity of care. It signals a turning point: a nationwide shift toward unified health records and citizen-centric services. Yet, Dr Soumya underscored critical gaps that must be filled: robust primary healthcare systems, population-level data that is reliable, a trained public health workforce, and research capacity that keeps pace with innovation.
India’s frontline health workers remain burdened with fragmented reporting and silos that weaken referral systems. To unlock real gains, the system must shift from input-focused reforms to outcome-driven, team-based integrated care that ensures continuity through district-level coordination and on-the-job mentoring.
Standardising and strengthening vital statistics — particularly mortality data — will be crucial. Timely, disaggregated health data, she said, is the only route to targeted planning and equitable outcomes in a country as diverse as India. With its scientific talent and digital advantage, India can set global benchmarks in ethically governed, locally relevant health technologies.
Dr Soumya made a compelling case for philanthropy as the risk-taker India needs — supporting high-impact early-stage research, bridging innovation gaps, aligning capital with national health priorities, and enabling ecosystems that accelerate ideas into implementation. The urgency, she reminded the audience, could not be clearer: the world still lacks an effective vaccine for Tuberculosis, a disease that remains one of India’s most persistent killers.
The PIC–Wipro Lecture Series reinforced that health innovation is no longer a matter of scientific ambition, but national resilience. A future where disruptive technologies serve every Indian — regardless of income or location — will demand strong public institutions, visionary private sector engagement, and a relentless focus on equity. As Dr Soumya Swaminathan concluded, “It is the bridge built on research, context, and ethics that converts innovation into real, impactful health outcomes.”
India is now poised to build that bridge — not just for itself, but for the world.
Suchetana Choudhury
(suchetana.choudhuri@agrospectrumindia.com)